Understanding Low White Blood Cells (WBCS) in Communities of Color: Questions to Ask Your Doctor About Duffy-Null Associated Neutrophil Count (DANC)
September 04, 2024
White blood cells (WBC), or leukocytes, are part of the body's immune system and help fight infection and disease. Neutrophils are a type of leukocyte. They are a subset of granulocytes, along with eosinophils and basophils. Granulocyte means it's a type of white blood cell that contains granules in its cytoplasm. The granules are small particles that contain enzymes and other proteins that help the cell perform its specific functions in the immune response.
Neutrophils make up 50–70% of circulating leukocytes and are the first line of defense against bacterial infections. Neutrophils are the most common cells to arrive at the site of an infection or injury. They recognize foreign antigens (molecules the immune system recognizes as potentially harmful) and phagocytose (remove them by ingestion/engulfing) them.
At the onset of an infection neutrophil count often increases as a part of the immune system's immediate response. As the infection progresses, the neutrophil count can fluctuate. Neutrophil count may be low when the infection is severe or prolonged or if the person has an underlying condition affecting neutrophil production. Perpetually, low neutrophils can increase one’s risk of infection and can be an indication of a compromised immune system.
Neutropenia (low neutrophils) is defined by an absolute neutrophil count (ANC) <1500/microL in most populations. However, it has been demonstrated that a large number of otherwise healthy people of color have low ANC in comparison to those of European descent. This is called Duffy-null associated neutrophil count (DANC; formerly called benign ethnic neutropenia; also called constitutional neutropenia) and is an inherited condition.
People with this condition do not have recurrent or severe infections the way people with neutropenia typically do. DANC most often presents in people of African descent, Sephardic Jews, West Indians, Yemenites, Greeks, and Arabs. And it’s estimated that 25-50% of African Americans have DANC.
Key characteristics of DANC:
- Genetic basis: DANC is linked to a single nucleotide polymorphism (a common genetic variation where a single "letter" in the DNA sequence differs from what's typically found at that position in most people) in the promoter region of the ACKR1 gene (a specific DNA sequence located upstream of the gene that controls when and how much the gene is expressed, particularly in red blood cells; formerly known as DARC), which results in the Duffy-null phenotype.
The Duffy-null variation:
In some people, there's a SNP in the promoter region of the ACKR1 gene. This tiny change is like flipping the "ON" switch to "OFF".
Because of this change, the body doesn't make the Duffy antigen protein. It's as if the instruction manual for this protein is never opened. The Duffy antigen protein is located on the surface of red blood cells and on other tissues and has several important functions, some of which are:
- Acting as a receptor for chemokines, which are small proteins that guide the movement of immune cells like neutrophils. It helps control the levels and distribution of these chemokines in the body.
- Influences neutrophil migration, helping direct neutrophils to sites of inflammation.
- The Duffy antigen on red blood cells is thought to act as a "sink" for inflammatory chemokines, potentially dampening excessive inflammatory responses.
- The Duffy antigen on endothelial cells may promote leukocyte (including neutrophil) diapedesis - the process of cells moving through the walls of blood vessels.
- It also acts as a receptor for the parasites responsible for malaria; so when the body doesn’t make the Duffy antigen protein it’s protective against some malaria types because the parasite can’t bind.
When people have this genetic variation and don't produce the Duffy antigen, we say they have the "Duffy-null phenotype". Phenotype just means the observable characteristics resulting from a person's genes.
Prevalence: Approximately 66.7% of Black individuals have the Duffy-null phenotype (you can have the phenotype without having DANC). Having the Duffy-null phenotype does not automatically mean an individual will have a low neutrophil count (DANC).
ANC differences: There is a significant difference in absolute neutrophil counts (ANCs) between Duffy-null and Duffy non-null individuals. The median ANC for Duffy-null individuals is 2820 cells per μL, compared to 5005 cells per μL for Duffy non-null individuals.
Lower ANC threshold: About 23.8% of Duffy-null individuals have an ANC below 2000 cells per μL, which is often considered the lower limit of normal in many reference ranges.
Clinical significance: Despite the lower ANC, individuals with DANC do not have an increased risk of infection. They have normal bone marrow cellularity (percentage of bone marrow volume made up of stem cells that will turn into red and white blood cells, including neutrophils), maturation, and a robust response to infection. This means, the bone marrow of individuals with DANC functions normally in producing blood cells, including neutrophils. The lower circulating neutrophil count is not due to decreased production but rather due to differences in neutrophil distribution in the body. In people with DANC, more neutrophils might be sticking to the walls of blood vessels, hanging out in certain tissues or organs or moving between the blood and tissues differently than in people without DANC. Their bodies still have enough neutrophils; they're just not all floating freely in the bloodstream where we typically count them.
Implications:
The existence of DANC highlights the need for Duffy-null-specific ANC reference ranges. By using standard references many healthy Duffy-null individuals may be incorrectly labeled as having neutropenia, leading to unnecessary medical and potentially invasive interventions and procedures, like bone marrow biopsies (a special hollow needle is inserted through the skin and into the bone to collect a sample) or the discontinuation of critical medications (e.g. the antipsychotic Clozapine, rheumatology medications, and certain cancer medications that cause neutropenia) in Duffy-null individuals. Delayed treatment, especially in cancer care because of concerns about “low” neutrophil counts.
Recognizing DANC is crucial for providing appropriate care and avoiding potential iatrogenic (introduced by medicine) harm due to misinterpretation of ANC values. Furthermore, since the Duffy-null phenotype is more common in certain populations (e.g., individuals of African or Middle Eastern descent), using inappropriate reference ranges can contribute to health disparities.
Other reasons for low WBC:
- Nutritional deficiencies: Lack of certain vitamins and minerals, especially vitamin B12 and folate, can lead to neutropenia.
- Viral infections: Common viruses like influenza, Epstein-Barr virus, and HIV can lower neutrophil counts.
- Severe bacterial infections: Some serious infections can use up neutrophils faster than the body can produce them.
- Autoimmune disorders: Conditions like lupus or rheumatoid arthritis can cause the immune system to attack and destroy neutrophils.
- Bone marrow disorders: Diseases affecting the bone marrow, where neutrophils are produced, can result in neutropenia.
- Inherited conditions: Some rare genetic disorders can cause chronic neutropenia from birth.
- Radiation exposure: High doses of radiation can damage bone marrow and reduce neutrophil production.
- Alcohol abuse: Excessive alcohol consumption can interfere with neutrophil production and function.
- Certain medications: Some drugs, including antibiotics and psychiatric medications, can cause neutropenia as a side effect.
Testing can provide clarity about whether a person has DANC or if there is a clinical reason for their neutropenia:
- Complete Blood Count (CBC) with differential: This blood test measures the neutrophil count. This is typically the first test done to confirm neutropenia and assess other blood cell counts.
- Blood smear: A microscopic examination of blood cells to assess their appearance and numbers.
- Genetic testing: This detects the normal variation in the ACKR1 gene associated with DANC. May also be done for suspected congenital neutropenias, such as sequencing the ELANE gene for cyclic neutropenia (repetitive/cyclical episodes of low neutrophils).
- Bone marrow examination: This involves taking a sample of bone marrow to examine under a microscope. It helps determine if neutrophil production is normal or if there are issues with cell maturation or stem cell numbers.
- Nutritional tests: Measurements of vitamin B12, folate, and copper levels can help identify nutritional deficiencies causing neutropenia.
- Autoimmune tests: Antinuclear antibody (ANA) and rheumatoid factor tests can screen for underlying autoimmune disorders.
- Flow cytometry: This can be used to evaluate for large granular lymphocyte (LGL) syndrome, even without obvious lymphocytosis.
- HIV testing: All patients with unexplained neutropenia should be tested for HIV.
- Immunological screening: Tests for immunoglobulin levels or T-cell subsets may be done if immunodeficiency disorders are suspected.
- Antineutrophil antibody tests: These can be performed if immune neutropenia is suspected, though they're not always reliable or widely available.
- Specific tests for suspected infections: This may include cultures or serological tests for viruses, bacteria, or other pathogens that can cause neutropenia.
The CBC with differential is a standard, widely-used test that's most likely to be routinely covered by insurance plans for evaluating blood disorders or unexplained symptoms related to blood cell abnormalities. Other tests like genetic testing, bone marrow examination, or specialized immunological screenings may require additional justification for insurance coverage.
DANC is a normal variation, not a disease.
It’s important to know your blood work trends! If you’ve noticed that your neutrophils are consistently flagged as low, consider asking your doctor some questions:
Can we test for the Duffy-null phenotype or genotype? This could involve genetic testing for the ACKR1 gene variation or a special blood typing test.
How do my neutrophil counts compare to Duffy-null specific reference ranges?
Standard reference ranges may not be appropriate for individuals with DANC.
Is my lower neutrophil count clinically significant, given the possibility of DANC?
DANC is considered a normal variation, not a disease.
Are there any additional tests we should consider to rule out other causes of neutropenia? This might include a complete blood count (CBC) with differential or a blood smear.
How might DANC impact my medical care or treatment decisions in the future? This could affect interpretation of blood tests or decisions about certain medications.
Should I carry documentation about my DANC status to share with other healthcare providers? This can help prevent misdiagnosis or unnecessary testing in the future.
Are there any situations where I should be more concerned about my neutrophil counts? Understanding when to seek medical attention is important.
Could DANC impact my eligibility for certain clinical trials or treatments? Some trials or treatments have neutrophil count cutoffs that may need to be adjusted.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2628742/
https://www-uptodate-com.une.idm.oclc.org/contents/overview-of-neutropenia-in-children-and-adolescents?search=low%20wbc%20count%20in%20african%20americans&source=search_result&selectedTitle=2%7E150&usage_type=default&display_rank=2
https://www.webmd.com/cancer/white-blood-cell-count-low
https://ashpublications.org/bloodadvances/article/7/3/317/486360/Absolute-neutrophil-count-by-Duffy-status-among
Leave a comment
Comments will be approved before showing up.
Also in Iwilla Remedy Herbalism & Spirituality Blog
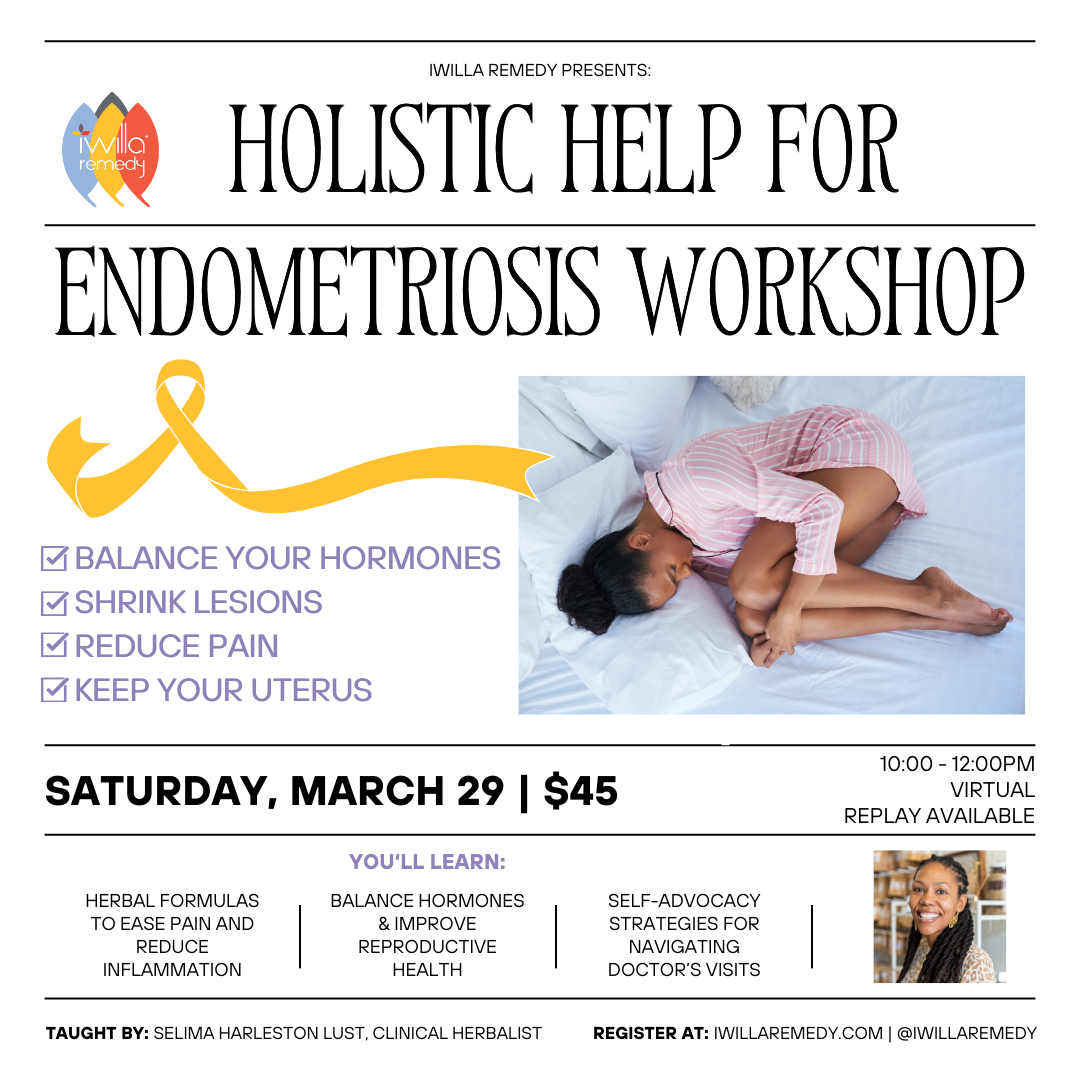
Holistic Help for Endometriosis Workshop
March 10, 2025
Struggling with endometriosis? You’re not alone. Join this empowering workshop to learn holistic strategies that support your body, ease pain, and promote healing. Discover how to balance hormones, reduce inflammation, and use herbs, nutrition, and lifestyle practices to reclaim your quality of life. You’ll also gain tools for self-advocacy and navigating medical care. It’s time to work with your body—not against it.

Herbal Business Finances? Do THIS!
February 17, 2025
Simple, stress-free financial systems to help you manage your bills, track cash flow, and take control of your herbal business—all for FREE!

Everything you need to know about the Herbalism Conference
February 13, 2025
The 2025 Virtual Herbalism Conference is happening February 16-21, and I’d love for you to join me! This event is entirely FREE and brings together 30+ of the world’s leading herbalists, educators, and visionaries to celebrate connections – connections to plants, to one another, and to the practices that nourish us all.
Store Hours
Monday: 10:00 AM - 6:00 PM
Tuesday: 10:00 AM - 6:00 PM
Wednesday: Closed
Thursday: 10:00 AM - 2:00 PM
Friday: By Appointment
Saturday & Sunday: Closed
2752 E. Ponce de Leon Ave. Suite I Decatur, GA 30030
(347) 414-7354
Navigation
© 2025 Iwilla Remedy. | 2752 E. Ponce de Leon Ave. Suite I Decatur, GA 30030 | Powered by Shopify